What is persistent pain?
However, for some people, even though the injury has healed, the pain can continue and become persistent. For others, persistent pain can start without any obvious cause. Ongoing pain is not usually related to bodily tissues, but rather to changes within the nervous system. When the nervous system becomes more alert, it is more sensitive, therefore usual activities become more challenging which can lead to distress and loss of function.
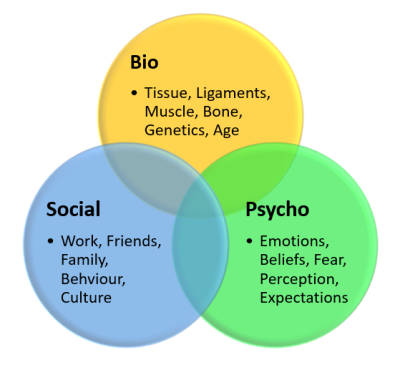
Traditionally, treatments for chronic pain were tissue based; this approach is known as the biomedical model. However, the benefits of treatments that target the tissues are often short lived, or non-existent. Taking a different approach to supporting people with persistent pain, known as the biopsychosocial approach, has been shown to be much more effective in improving peoples’ quality of life. This approach considers how we feel, what we think and what we do, and gives the opportunity to manage chronic pain more successfully. This approach can reduce the ‘volume’ of pain produced by the nervous system, allowing people to lead more fulfilling lives.
Live well with pain
Live Well with Pain is run by an alliance of healthcare professionals working in pain management and people with lived experience of persistent pain.
They share a passionate belief in the power of self-management to improve life for people with pain.
By combining their professional and personal experience they have developed a range of self-management resources that have been tried and tested over many years, such as a leaflet titled "Ten Footsteps to Living Well with Pain".
They have built this Live Well with Pain website to share these resources with others.
Why things hurt
In this video, Lorimer Moseley, a Pain Scientist and Physiotherapist, explores the view that the pain we feel is our bodies' way of protecting us from damaging tissues further. He also looks at what this might mean for those who suffer from chronic pain.
Tame the Beast
Pain scientists are starting to think differently about pain and its causes.
And they're making exciting discoveries…
To find out more information, you can visit the Tame the Beast website which has more information on understanding your pain and useful resources that may help you.
Understanding Pain
Here is an easy to follow video about chronic pain. It helps you understand what current research has been saying about chronic pain - that it's not a joint or muscle problem, rather a 're-wiring' of the brain perception of itself. In other words, the brain has become more sensitive than before.
Summary
There is a lot of information out there for people suffering with chronic pain. For a summary of the information on this website, you can download our summary sheet, which contains links to some of the information you may find useful.
Supported self-management
Understandably, living with pain can have a significant impact on your functioning, mood and overall quality of life.
Research has found that managing the overall experience of pain, including mood and functioning, rather than just the pain itself, is more effective in improving physical functioning and pain.
Listed below are some practical strategies you can use to support various different areas of your life which may be impacted by living with pain.
However, living with pain can be overwhelming and it can be hard to know where to start, so here is a tool to help you get started on the Live Well with Pain website.
When living with persistent pain, your priorities can understandably change to focusing more on what needs to be done, rather than focusing on what you would like to do.
This can often mean that you may prioritise the things you need to do over the things that you do for enjoyment. It can be difficult to feel as though you have enough time, or the ability, to do the things that you might want to do. Setting achievable goals to support you to break down activities can be a helpful way to reintroduce valued activities back into your life.
Before writing down your goal, think about the following questions:
- Is your goal something rewarding/valued to you personally? For example, it is not focused on the needs of someone else
- Is it realistic? – In the time that you have given yourself, will you realistically be able to work towards this goal?
- How confident are you with setting this goal? It is good to gauge this out of 10, with 10 being extremely confident and 1 being no confidence at all in achieving the goal. Ideally, this should be at 5 and above.
Below are some questions to help you start thinking about what is important to you. You can download these questions as a goal setting worksheet to print out and fill in:
- The first short-term goal I will achieve is
- When do I start? set yourself a start date and a proposed end date
- Who can help me? List family members, friends and co-workers who can help you meet your goals. Preferably have at least 1 person who will encourage you if the going gets tough:
- What resources will I need to meet my goal?
- What possible obstacles could get in my way?
- What will help me overcome any obstacles?
The goal ladder below is a nice visual aid to help you work towards your goal. Write your goal at the top of the ladder and use the rungs below to break down the steps you might take towards your goal.
It is very common for people with persistent pain to have difficulties with sleep. This can be getting off to sleep, disturbed sleep or not feeling rested after sleep. There are different stages of sleep. Our body and mind recovers, heals and rests in the deeper stages of sleep. When someone has persistent pain their nervous system is sensitised making it harder for that person to go into a deep sleep.
The circadian rhythm is your body's internal body clock and when properly aligned, it promotes restorative sleep. When the circadian rhythm is out of sync, it can contribute to sleep problems. Applying good sleep hygiene (focused on sleep behaviour and your environment) can help optimise the circadian rhythm, thereby increasing the likelihood of good sleep. The following points are some healthy changes that can make a difference to your sleep and wellbeing:
- Spend some time in natural light during the day
- Try to maintain your levels of activity during the day
- Avoid stimulating food or activities 6-8 hours prior to bed (food, alcohol, screen time)
- Stick to a regular routine (waking up, eating and bed time,)
- Take part in relaxing, calming activities prior to bed
- Ensure your bedroom environment is cool, quiet and dark
There is more information on the Sleep Council website, or see this sleep document regarding pain and sleep.
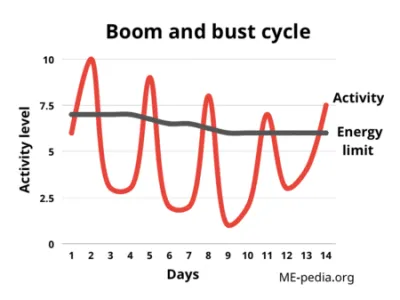
Pacing is not always about doing less. Sometimes, it is good to think of pacing in terms of how much energy you have to use during the day, and how is the best and most efficient way to use this. Most people fall into one of two categories: either doing too much or doing too little. There can be consequences of either overdoing or underdoing activities that you did not intend to occur. For example, it can bring about, a flare up of your pain, or mean that you’re unable to do the things you want to do. You may have noticed that a flare up can take days or even weeks to settle back down. During this time, you are likely to be less physically active, meaning you may be missing out on enjoyable activities, having time out of work and being unable to complete daily tasks that are important to you.
When your experience of pain settles, it is not uncommon to feel tempted to catch up on the activities you might have missed whilst you were managing an increase in your pain. This increase in activity can itself contribute to a flare up, repeating this cycle again. We use the term ‘boom-bust cycle’ to describe this pattern.
It can be helpful to see how active / inactive you are by keeping an Activity Diary. Using a diary can encourage us to be reflective about the amount of activity that we are actually doing each day. When you have an idea of your energy levels throughout the day, you can start putting strategies in place to manage this better.
The Traffic Light System Tool can also be a useful tool to help categorise certain activities to help you pace them throughout the day. This tool helps you categorise your activity levels into:
- “Activities that definitely make your pain worse, or make you feel more stressed / agitated” which are marked as RED activities
- “Activities that are borderline and vary” which are marked as AMBER activities
- “Activities that don’t make your pain worse, or make YOU feel better” which are GREEN activities
The most effective way of managing energy levels is for your day to have a combination of all 3 of these throughout the day.
We will all have some tasks that are classed as a red activity, however if your day is all red activities then this will likely impact your experience of pain. If we approach red tasks in combination with green activities this can help you to manage your pain by balancing out the types of activity you are doing throughout the day.
The activities you do should be performed to your personal tolerable pain levels. This means it will vary between individuals and you should only go as far as is reasonably comfortable for you. This may include slower and smaller movements. If you are unsure on what activity to do or how much, please speak to a health care professional first.
Have you ever been told to “relax” or “just breathe”?
Our breath is the one automatic bodily function that we have conscious control over. We hold a lot emotion in our breath, for example, you may ‘gasp’ in shock or hold your breath when in pain. It is also common to breathe shallowly when you are in pain, triggering the sympathetic nervous system further. Tapping into our breath as a form of relaxation has been shown to boost the parasympathetic nervous system, which in turn can help your pain experience.
Here are a variety of relaxation techniques, all of which are aimed at slowing us down. Some are breathing orientated, while others involve visualisation and muscle relaxation.
Full video
Diaphragmatic breathing
Square breathing
5 Finger technique
Progressive muscle relaxation
Heartmath breathing
Guided imagery and visualisation
Mindfulness of breath
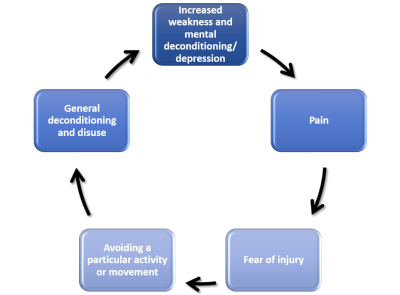
There is significant evidence to suggest that maintaining a level of activity is part of good pain management. This does not have to mean going to the gym or out for a run, activities such as chores around the house or looking after others are all tasks that use our muscles and joints. When we become less active our bodies decondition (see picture below) and this can amplify our pain. Over time, our nervous system can become more sensitive to movement so physical tasks become more of a struggle. Most people will say that they are less active now but their pain has still worsened.
It doesn’t really matter what form of activity you do, any movement is good. For example, studies have found that housework chores can burn up to 315 calories an hour. Tai chi, although a more formal type of activity, has been found to reduce pain and increase function and mood for those who experience persistent pain. You can try Tai Chi for yourself as we have created two videos, one that is a warm up, that is practised on our pain management programme, and should be done first, and one that uses the form from our tai chi class. Some prefer a more structured approach like these seated exercises or static exercises like in this poster from Versus Arthritis.
If you are unsure of what activity to do or how much, please speak to a health care professional first. It is normal to experience some discomfort when doing exercises, and individuals may start at different points. Pain should not increase excessively during or immediately after the activity. Discomfort should return to pre-activity levels 24-48 hours after the activity has finished.
These exercises/activities should be performed to your personal tolerable pain levels. This means it will vary between individuals and you should only go as far as is reasonably comfortable for you. This may include slower and smaller movements.
If you would like some exercises for specific joint or body parts, please visit the Musculoskeletal (MSK) Service's webpages where you will find information on various conditions and ways to self manage.
The evidence suggests that a multifactorial approach to managing chronic pain is much more effective than one treatment alone. Unfortunately, medicines alone rarely offer more than a modest reduction in chronic pain but they do have their place. It is important to ask yourself “what are my medicines doing for my pain?”
Below are a selection of videos explaining the role and use of different medications in managing chronic pain.
A Patient's Experience of Medication
A 5 News investigation reveals that thousands of people, struggling with long-term pain, have been taking addictive medicines for years, when experts say they're only really effective for a few months. Louise Trewern, who relied on the painkillers for 12 years, tells 5 News: “I was shocked to find my pain improved from being off the drugs”.
Paracetamol
Paracetamol is a medicine used to treat mild to moderate pain. In this video, Peter Farley (Pharmacist for the Chronic Pain Management Service) talks about when these medicines are best used, how to take them, and the dose that is recommended.
Anti-inflammatories
Anti-inflammatory drugs, also known as NSAIDs (Non-Steroidal Anti-Inflammatory Drugs), are used to reduce pain and inflammation. Peter Farley (Pharmacist for the Chronic Pain Management Service) talks about when these medicines are best used, how to take them, and the dose that is recommended.
Neuropathic pain
Neuropathic pain medications work by affecting the nervous system to reduce sensitivity and pain signals. Peter Farley (Pharmacist for the Chronic Pain Management Service) talks about when these medicines are best used, how to take them, and the dose that is recommended.
Opioids
Prescription Opioid medications are mainly used for the treatment of pain. Peter Farley (Pharmacist for the Chronic Pain Management Service) talks about when these medicines are best used, how to take them, and the dose that is recommended.
If your goal is related to going out more or building confidence, below are some links for local groups that may be helpful.
Therapeutic learning activities with animals, plants, creativity and the countryside for people recovering from mental ill health. Therapeutic learning activities with animals, plants, creativity and the countryside for people recovering from mental ill health.
Age UK and our partner charity The Silver Line offer free telephone friendship services so you can enjoy chatting with someone over the phone, all from the comfort of your own home.
Whether you’d like to speak to someone every week, or just want to talk when the need strikes, we’re here to help.
Midlands Partnership University NHS Foundation Trust Wellbeing & Recovery College
The Wellbeing and Recovery College provides recovery-focused education courses that are accessible to everyone in our local communities. We work together to create an environment of hope, control and opportunity for us all.
Staffordshire Connects is a social support hub for activities, support, and advice for people in Staffordshire
Commissioned by Staffordshire County Council, we are here to help with every aspect of health, fitness and wellbeing, with all of our FREE programmes proven to have long term benefits. Commissioned by Staffordshire County Council, we are here to help with every aspect of health, fitness and wellbeing, with all of our FREE programmes proven to have long term benefits.
Whether you want to feel fitter, lose weight or quit smoking we're here to help the people of Derbyshire to Live Life Better. Whatever your goal, you'll be amazed how a little extra support and advice can make a big difference.
Support We Offer
The chronic pain management team takes a multidisciplinary approach. This is because persistent pain impacts people in different ways and one size does not fit all. Our team involves pain consultants, Clinical Psychologists, specialist physiotherapists and a pharmacist who specialises in pain medications. Alongside traditional one-to-one appointments, you may be offered the chance to access one our group sessions including the Pain Management Program, Achieving Balance Group, or Tai Chi.
The following information shows how our team works together with you, to offer pain education and support that is tailored to your individual needs to help you manage your pain.
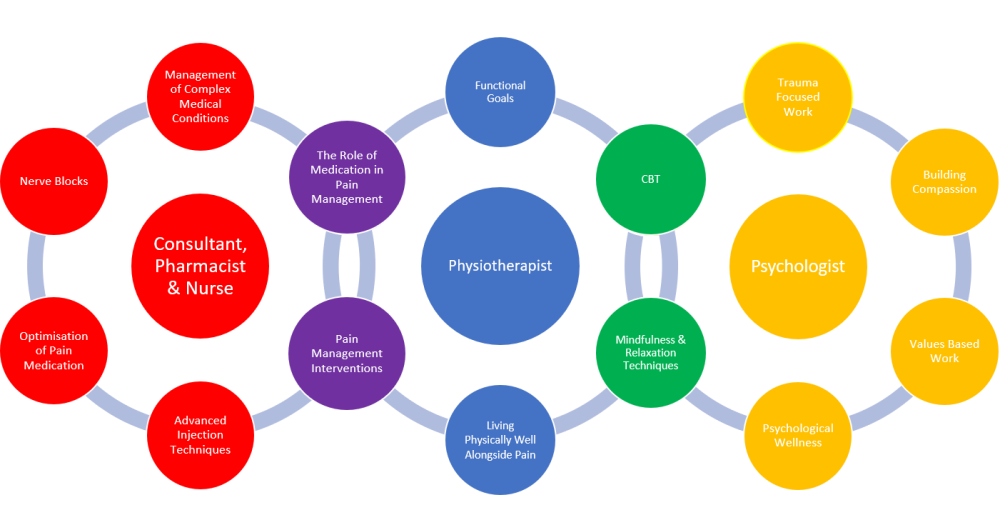
The role of each member of our team
Our physiotherapists can help you to:
- Understand persistent pain and what involvement the nervous system has with our pain
- Come to terms with long term pain
- Understand how to manage your daily life and demands with persistent pain (pacing)
- Set valued goals to work towards the things in life that pain is currently having an impact on e.g. hobbies, work
- Be active with persistent pain
- Sleep when you live with persistent pain
- Incorporate evidenced techniques like relaxation and mindfulness to help manage pain.
- Manage setbacks (also known as flare ups) when you have persistent pain
Our specialist Pain Consultants can offer a wide range of advanced treatment techniques that include:
- Injections
- Medication reviews
- Denervation techniques
Our pharmacist has years of experience helping people with persistent pain to:
- Optimise medical management
- Understand the role of medication in your management
Psychologists working in pain services aim to:
- Support people to understand and manage the impact that living with persistent pain can have on their emotional wellbeing
- Help people to live meaningfully alongside their experience of pain
- Help you to think about how pain affects various different areas of your life, and the changes that you might like to make to this
Some examples of this might include returning to previously enjoyed activities, improving the relationships and connections you have with the people around you, or spending time talking through and working towards accepting the journey you have been on in relation to your experience of pain.
The chronic pain nurse is an independent professional who is a part of multi-professional team. This role includes the following:
- Conducting Qutenza clinics for the treatment of chronic focal neuropathic pain
- Providing holistic follow-up sessions for all interventions such as injections, nerve blocks.
- Acting as patient’s case co-ordinator, communicating with the team, attending the multi-professional treatment team meetings.
- Assisting with complex case interventions such as cervical facet joints denervation in outpatient clinics.
- Reviewing the patient’s progress, helping with evaluating and monitoring the treatment outcomes, educating the patients with medicines, self-management, group therapy programmes when appropriate.
- Supporting or leading service evaluation, audit and research projects within the pain management service
Groups
Below is more information on the groups that are offered within the Chronic Pain Management Service.
The Pain Management Program (PMP) is a 6 week education program, for 3 hours per week. There is NO role play within the group, you are free to share your experiences if you wish, but you don't have to.
You will be referred into the program following a discussion with someone in the service. The groups take place in various locations, at either Burton, Lichfield or Stonydelph. More information on clinic locations can be found on our My Appointment section.
The aim of the program is to promote self-management strategies to reduce the impact of chronic pain and to improve your quality of life. It also offers you the opportunity to:
- Meet others with chronic pain
- Improve your understanding of chronic pain
- Help you manage the distress associated with pain
- Increase your confidence in being able to do things
To get the most out of PMP you need to be:
- Open minded
- Prepared to take ownership of your pain management
- Ready to identify and challenge unhelpful ways of managing your pain
- Ready to set realistic goals
- In a position to make changes
More information about the PMP can be found on our What is a Pain Management Programme (patient information leaflet)
The group is based on a Compassion Focused Therapy approach. The aim of the group is to explore an understanding of our emotional systems and how they are affected when living with a long-term health condition. The group aims to support the building of skills and strategies to respond to health challenges from a more Compassionate stance, developing skills to bring balance to the emotional systems by increasing soothing, down regulating the body’s threat system and also overcoming barriers to manageable goals. The Compassion for Living with Persistent Pain Group is delivered in weekly sessions for 8 weeks. Each session will last up to 2 hours. The group is currently delivered in a virtual group setting.
More information about the Compassion for Living with Persistent Pain Group can be found in the Compassion for Living with Persistent Pain Group (patient information leaflet)
Tai Chi Chuan is a suitable form of exercise for many people with chronic pain. It is gentle, involving slow, smooth, flowing movements which can help to quieten the mind and bring physical benefits. Tai Chi offers a way of improving pain, physical ability, relaxation and your general sense of well-being.
Tai Chi classes run for 6 weeks on a weekly basis, and you are expected to attend all 6 sessions. Sessions last for 1 hour. During the class, there will be opportunities for frequent breaks. To get the most out of the class, you will need to practice for a short time each day at home.
Tai Chi does not require any special equipment, but please come dressed in comfortable loose clothing, and footwear that is appropriate for some gentle physical activity (flat and closed-in, without a flared heel is best). Please bring a drink of water with you.
You will be asked to complete a short questionnaire before you join the class, and again at the end. This will allow us to monitor your progress, as well as the effectiveness of the class.
You will also be asked to complete a short feedback form at the end of the course. This is anonymous and will be used to improve our service to patients.